Finding Your Path ~ Back to School for TSW Warrior
Back to school in Topical Steroid Withdrawal can be so much better when you know that you will be understood, you will be safe, you will find support when you need it and opportunities to learn and grow in new and brave ways. I mean this for your child in TSW. I mean this for you. Whether it is your first back to school in TSW, or if it is like ours, your fifth, each warrior is on their own unique path towards healing and thriving. Wherever you are as back to school approaches this year, or if you have already started, know that it is ok to be different as you identify your strengths, and advocate for your health and learning needs.
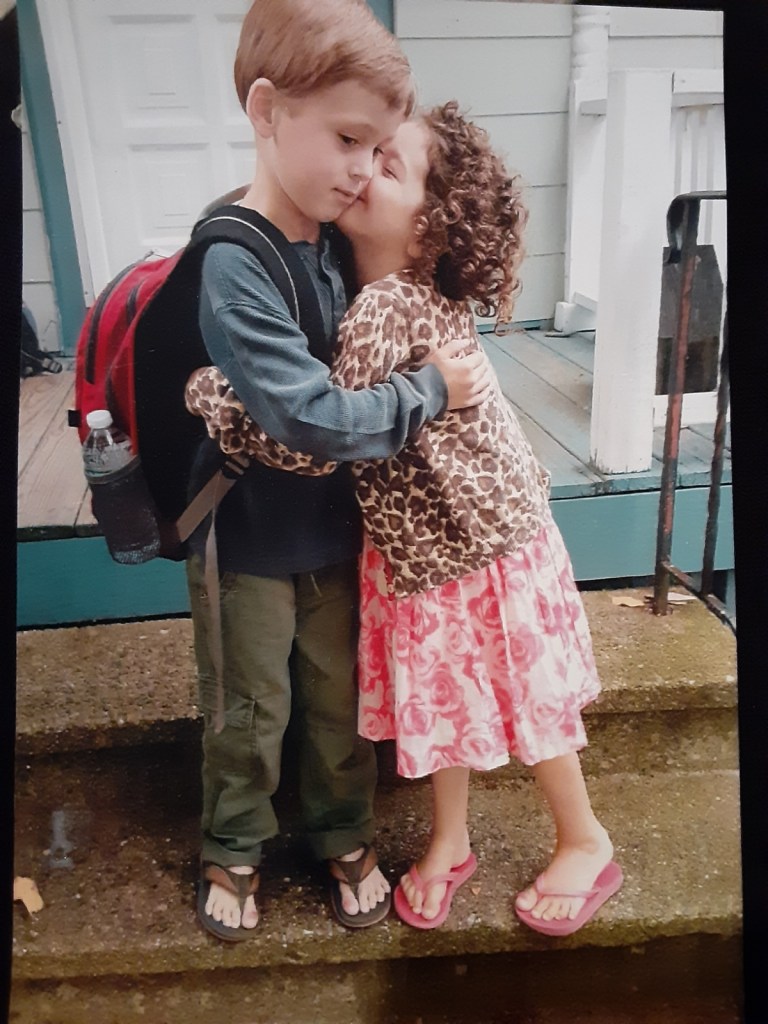
Five years ago, when my son Max was 15 months TSW, and about to start Kindergarten, I so wanted him to be part of the familiar path his classmates would be on. I didn’t know up to the start of school, if he should be home-schooled or not, with the intensity of his TSW symptoms. His school team was incredible but his first day was heartbreaking. The severity of the nerve and itch episode hurt emotionally and physically. Max was only able to attend Kindergarten in the afternoons due to exhaustion and pain from skin setbacks after scratching arms and legs at school. I was called into the nurse’s office each day (a plan we were grateful to have with the school though it meant deep stretching on one income), and Max would come home after the nerve pain and itch episode to sleep and recover. It was our attempt to stay on the same path as others, but it wasn’t the right route for us then.
We took Max out of school in January 2016, and kept him home to rest and heal. He spent months on the couch. Anything that dilated his blood vessels (fatigue, heat, stress, digestion, fragrance), would trigger nerve pain and itch. Those different, not school days, allowed his healing needs to lead the way. He could sleep in after a night of being up. We could bundle up on a good afternoon and drive to the beach to explore rocks. The right path meant trusting that what felt like loss would lead to gain. Max attended first grade full time. I was on call for the intense and almost daily nerve pain and itch episodes, but he would return to class afterwards. Each school year brought more healing and learning. Max will soon start his fourth grade year and he loves school. We have seen so many gains each new school year and will share how we planned and persevered!
The Planning – Know Your Rights
Section 504 of the Rehabilitation Act of 1973 is an important legal right for your child. Section 504 requires that public K-12 schools provide a free appropriate education (FAPE), to students who qualify due to a physical or mental impairment. If your child attends a school that receives federal funding they have the right to reasonable accommodations developed between the school, student and family in the form of a 504 plan. Meeting and speaking with your child’s educational team can feel overwhelming at first. Each year I try to prepare a written summary prior to the meeting. Having notes helps keep me on track during meetings when I have been nervous, exhausted, or felt emotional to review our health journey with new team members.
- Reach out to your school’s guidance counselor and/or IEP coordinator with a request in writing to meet with your child’s teacher, school nurse and principal. Explain that you would like your child to be evaluated under Section 504.
- Consider reaching out 1-2 weeks before the start of each new school year.
- Prepare a written summary of your child’s health history, include current health issues: how are days and nights?
- Bring a copy of office notes and records from recent medical appointments if you feel that they appropriately represent your child’s health condition.
- Print information related to TSW to share with the team. (ITSAN.org)
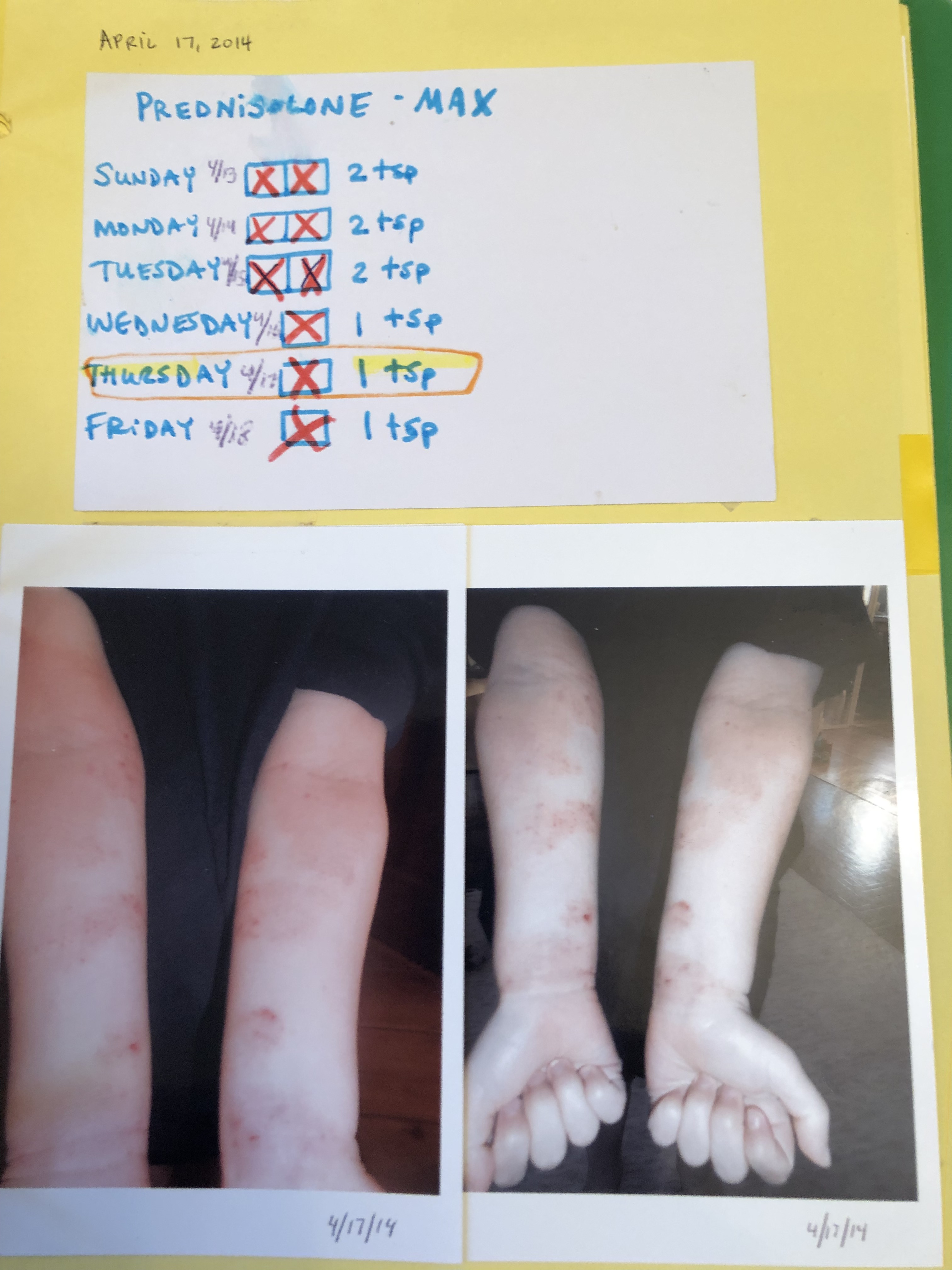
- Bring photos of your child in the beginning stages of TSW and the most recent photos of areas where healing is still occurring.
- Include your child in the process before the meeting by asking for their thoughts about going back to school and documenting their response.
- Develop a draft of accommodations you anticipate your child might need. (See below for examples).
- Consider and document your child’s strengths and your hopes for this school year.
- Keep breathing – it will be ok!
Additional thoughts: My son Max has many food, environmental and drug allergies so I request the meeting each year to develop his Health Plan and because TSW has been an ongoing physical health condition I also request a 504 Plan to develop classroom accommodations to support his specific physical needs. In the past I have brought a laptop computer to share pictures of Max. It is important to me that his team has a visual for areas still healing, such as his calves and feet, as the school nurse may be the only school provider to see these healing areas during the school year.
The 504 Plan Meeting – Getting to Know Your Warrior
Remember that you are likely not the first family your school has worked with dealing with a unique health issue. Great educators are open to learning and taking on new challenges in order to expand their skills and understanding. Your child’s educational team is there to help support you all in finding ways for your child to be successful in school.
- Thank your child’s team for the opportunity to meet.
- Inform the team that you have brought information to share about your child’s medical condition. Share a few words about your child’s strengths. Summarize your child’s health history and current health needs. Share photos of healing areas that may impact your child during the school day. Provide information about TSW. Share a copy of or read the thoughts and/or concerns your child has expressed about the school year.
- Discuss accommodations that may support your child accessing their education as they heal. For example, attending a partial school day if they are in need of additional time to rest/sleep/heal. Permission to wear comfy footwear for gym. Parent supplying cotton sheets to be used on the cot in the nurse’s office during a nerve pain and itch episode.
- Ask any questions including: What is the daily schedule? How many transitions do students have between classrooms and the building on a typical day? Discuss transportation planning including field trips.
Federal funds do not cover accommodations determined during a 504 Plan. Schools are required to cover the costs of reasonable accommodations through their own funds. Students and families are not required to cover the costs but being open to collaborating has been effective in our experience. We have donated a fan and provided supplies specific to Max’s needs when he has been in the nurse’s office. The school has provided a classroom with air conditioning when there was need and has offered a portable AC unit. Ongoing communication and planning with school providers has been excellent. The school went fragrance free in 2015 and it made such a difference.
Each year Max’s educational team has helped develop a 504 plan that reflects his current health needs. For example, his school nurse summarized: “Health Concern: Topical Steroid Withdrawal (TSW): causes skin to be red, burning, painful, intense itching, rashes, swelling and flaking skin. Thermoregulation altered. Fatigue and Insomnia. Accommodation/Intervention: When student is having an episode related to his TSW, he will have intense itching, pain and burning. Triggers may be emotional upset and physical activity at recess or PE, and feeling too hot or too cold. Student will stop activity as needed and will be allowed to take a break in a cooler space such as the RN office. Student will have liberal access to the nurse’s bathroom. Student may eat lunch in a quiet space, such as the RN office as needed. Sitting on the carpet can be difficult for student because of dust mite allergy and pain related to skin integrity. Student will have a chair in the classroom when needed. Student’s parent will be called during an episode, based on intensity and RN assessment, to assist student at school as needed or to take student home if appropriate.”
The school included a Safe Scratch Plan with language to replace, “Don’t scratch” or “Don’t itch” with encouragement like “Gentle rubs.” “This will get better.” “You are doing great.” “Let’s think about the next fun thing we are going to do.” The school nurse included a chart in Max’s Healthcare Plan to differentiate level of need and level of response between a “Mild episode of pruritus (itching) related to TSW” and a “Severe episode of pruritus.” Every team member including substitute teachers received a copy of the 504/Health plan and it became the “blueprint” for our path.
You will find your path and you will persevere!
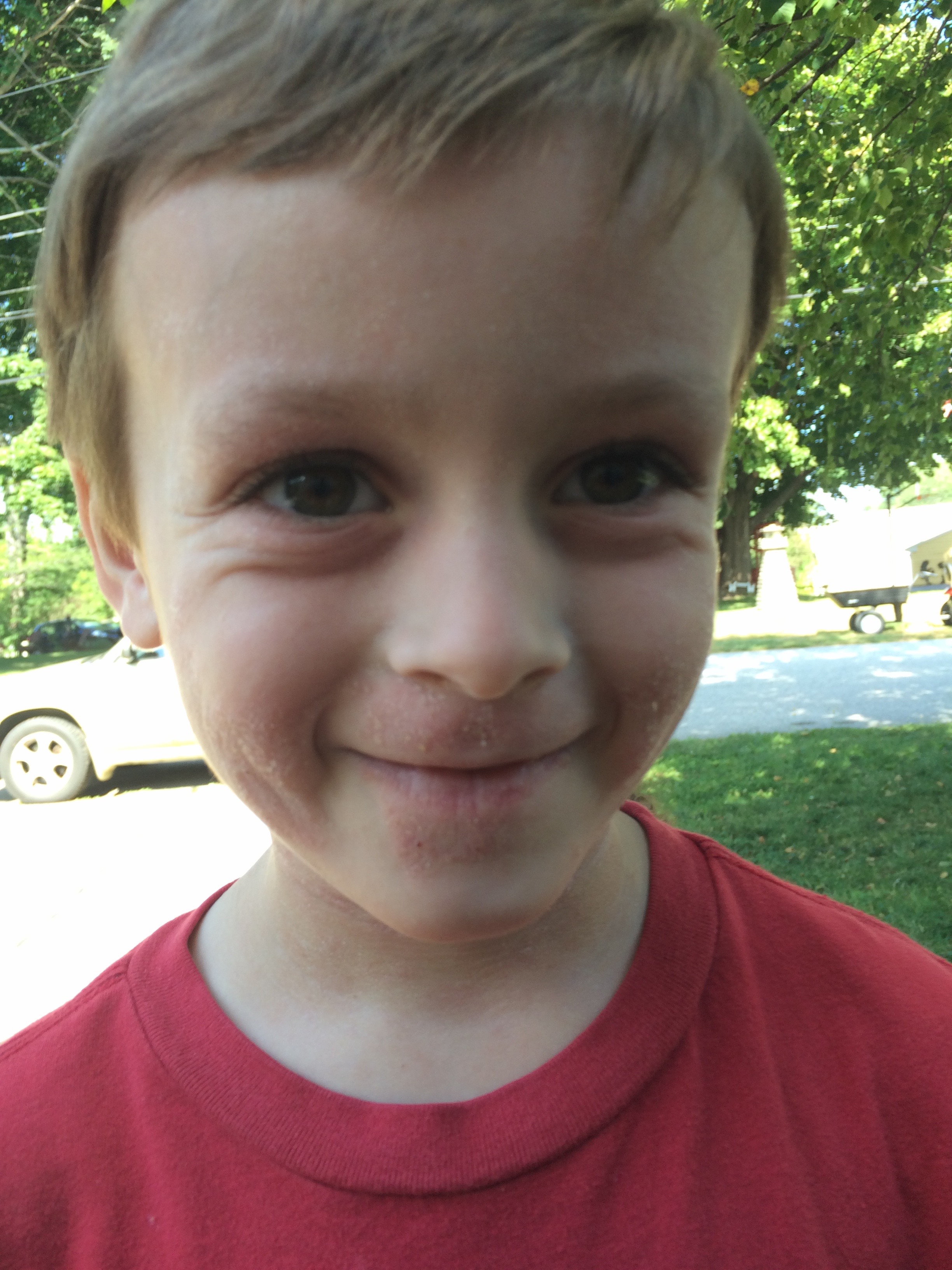
Back to School Words From Max (age 9) – To Your TSW Warrior
Max: Remember everything’s going to be ok. If you’re nervous, take a moment and then start. Focusing on a good thing and if you’re worrying about something, like that already happened or that’s coming, you can focus on what’s happening now. Deep breaths. And sometimes when I’m at recess I do yoga stretches. When you’re dealing with the itches you can just think helpful thoughts, maybe pull back for a sec, take a deep breath, maybe use the bathroom, try to lighten your itch, feel like a cloud, cause clouds are too fluffy to hurt themselves.
Me: What has improved since you started your first back to school in TSW?
Max: Whoa, I don’t break my skin. I don’t need to put Vaseline on before going into the tub. I used to itch really hard and start to bleed but now I barely itch at all and I barely break a scab.
Me: How has going back to school been during TSW?
Max: Well, I mean I have to thank it to my classmates, they’re so helpful with their understanding…in Kindergarten someone would always walk me down (to the nurse’s office), ask me if I was ok, everybody would ask the teacher if they could walk me down, they always wanted to…that was sort of funny. Now I can go down (to the nurse’s office) independently. Normally – put pressure and walk, sometimes run if it really itches, but I always slow down and take a deep breath so that my body doesn’t go too hyper and make everything more itchy than it is supposed to be.
Me: What has been helpful that your teachers have done?
Max: My teachers…if it is my arms they’d give me pressure and they’d tell me I could go down (to the nurse’s office) if I was itchy. They’d always be aware of what I was doing, like if I was beginning to get itchy, I would raise my hand, the teacher would look at me and point to the door. Itchy permission slip.
Me: What has been helpful from your nurse?
Max: My nurse is always…I’d ask for a washcloth and he’d always make it cold, that’s how I like my washcloths. He’d always tell me about something recent in science that I can listen to or a cool discovery that NASA has achieved or even some flashcards. I even got to see a trailer of a movie once.
Me: What has been helpful from your guidance counselor?
Max: She always says have a good day. She is cheerful.
Me: What has been helpful from your specials teachers?
Max: They always say I can go get a drink of water or go down to the nurse’s office. My gym teacher will always give me a positive answer and say I can go down to the nurse’s office and if I come back before the special ends he’s always happy.
Me: What has been helpful from your principal?
Max: My principal always understands what’s happening, she always waves and smiles. She gives me a thumbs up when I come out after itches. And every morning if I walk past her she’ll always wave and say, “Have a good day.” And when I tell her I haven’t had any itches all day she jumps and does a little Wooo-hooo!”
Me: Last words of advice for kids going back to school for the FIRST time in TSW?
Max: Never think about something bad, always think positive.
By Jolene MacDonald
Illustration by Max Duffy
Sources:
Francoeur, Esq, Laurel. How to Advocate for your Food Allergic Child
Jacqueline, Ilana. Surviving and Thriving with an Invisible Chronic Illness